Healey administration denies family’s request to place severely disabled woman at Wrentham Center
The Healey administration is refusing to admit a severely disabled woman to the state-run Wrentham Developmental Center even though state officials have been unable to find a suitable placement for her in any other residential setting.
As a result, Kristen Robinson, 50, who is profoundly intellectually disabled, blind, and quadriplegic, has been confined to Faulkner Hospital in Boston since early last month following a choking incident in her family’s home. She has seizure disorder and severe dysphagia, a medical condition that causes an inability to swallow.
Emails show that the Department of Developmental Services (DDS) denied a request by the hospital last month to discharge Kristen to the May Center, a medical unit at the Wrentham facility.
Kristen’s sisters and co-guardians, Kim Meehan and Karen Brady, want her to be admitted permanently to the Wrentham Center. They argue that Wrentham provides a higher and more comprehensive level of care than can be found in the DDS-funded, provider-based group home system.
Administration officials, however, have insisted that suitable settings for Kristen can be found in the group home system.
But the only group home identified so far by DDS as a possible setting for Kristen rejected her placement there in March because the home cannot accommodate residents in wheelchairs. In addition, as many as 25 nursing homes have indicated they would be unable to accommodate Kristen.
A clear case of need for an Intermediate Care Facility
Kristen had lived her entire life under her mother’s care in Walpole. But when their mother died last December, Kim and Karen and their husbands began to take turns caring for Kristen and staying overnight with her.
In a January 11 email to DDS Newton/South Norfolk Area Director Jane Fuller, Kim explained that her mother had died the previous month, and that Kristen needed a setting that would provide 24/7 nursing care due to her seizure and choking disorders. “Immediate help from DDS is necessary for Kristen’s safety and well being,” Kim wrote. “Please expedite the visit to WDC (the Wrentham Developmental Center)…”
Kim also said she and Karen are paying part of the cost of in-home care for Kristen out of pocket. She said that while Kristen needs 24/7 care, MassHealth is funding a maximum of only 10 hours a day of in-home services for her.
The Wrentham Developmental Center is an Intermediate Care Facility (ICF), which meets strict standards for care under the federal Medicaid Law. As we have reported, the administration has been allowing the census to drop at both the Wrentham Center and the Hogan Regional Center, the state’s only two remaining congregate ICFs.
A series of administrations has moved for decades to phase out state-run residential care for persons with intellectual and developmental disabilities (I/DD) in Massachusetts, and to replace it with contracted care in state-funded group homes. Nevertheless, we have long argued that the Wrentham and Hogan Centers provide a critical backstop for care for those persons with the most severe and profound levels of I/DD.
In an email last month, Fuller stated to Kim Meehan and Karen Brady that Kristen has “no right” to ICF care.
In our view, however, federal law and regulations do provide a right to ICF care to anyone who has been found to be eligible for that level of care, which is the case with Kristen.
Kim said the administration “is completely blocking Kristen’s right of choice of either an ICF or a community-based setting. DDS has given us no options for care in any setting,” she added.
Kristen’s case appears to be a clear case of the current administration’s improper refusal to offer an ICF placement to an individual who needs that level of care. It raises the question whether the administration has any consistent standard for admissions to ICF-level facilities.
Group home identified by DDS would not accept Kristen
Kim said that earlier this year, DDS began to look for a possible community-based placement for Kristen.
In March, DDS had identified a group home in Millis, operated by BAMSI, a DDS provider. But Kim said that when she, Karen, and an aide to her local state legislator, Representative John Rogers, arrived at the home with Kristen on March 20, the group home’s nurse said the residence couldn’t accommodate Kristen because she was in a wheelchair. The nurse said DDS had not informed her that Kristen was in a wheelchair and is quadriplegic.
Since then, Kim said, DDS has not identified any other potentially suitable group homes for Kristen. Since last month, she said, Faulkner Hospital has contacted as many as 25 nursing homes as possible placements for Kristen. None of those nursing facilities have apparently been able to accommodate her either. All have rejected her admission.
Ironically, the Healey administration recently promised to move 2,400 disabled persons out of nursing homes to settle a lawsuit alleging that those individuals had been improperly placed in nursing homes. That case follows the historic Rolland v. Cellucci lawsuit, which similarly resulted in the discharge of persons with I/DD from nursing homes in Massachusetts.
State officials suggested lowering bed to the floor
Kim said that despite Kristen’s limited ability to move, she can roll over and fall out of most nursing home beds. Nursing homes, in fact, are largely prohibited from using beds with side rails. That is one of many reasons, Kim maintained, that nursing homes are not appropriate settings for persons like Kristen with I/DD.
Yet, Healey administration officials are apparently not ruling nursing homes out in Kristen’s case. Kim said that in a meeting she had with ombudsmen from both DDS and the Executive Office of Health and Human Services (EOHHS), one state official suggested lowering Kristen’s bed to the floor, and placing mats nearby.
Kim said one of the many problems with that suggestion is that Kristen has pica, an eating disorder in which she will eat non-food items. “She will eat anything on the floor,” she said.
“Think about a 10-week-old,” Kim wrote to us in an email. “How they behave; what they are capable of. That is Kristen! I’m fighting hard with everything I have! I do not understand how my sister can be treated like this as a disabled person!”
DDS official claims, “No one has a ‘right’ to an ICF”
In a March 20 email to Kim, the same day that the BAMSI nurse stated that the Millis home couldn’t accommodate Kristen, Fuller first stated that, “No one has a “right” to an ICF.” She then asserted, directly after that statement, that, “DDS does not force anyone to accept services.”
It’s not clear what Fuller meant by the second statement, other than possibly implying that Kim and Karen would have to accept DDS’s position against ICF care if they wanted services at all for their sister.
DDS statement ignores federal law and regulations
In our view, Fuller’s claim that no one has a right to ICF care does not comply with the federal Medicaid law and regulations. Those rules require that ICFs be offered as a choice to all persons whose intellectual disability makes them eligible for care under the Medicaid Home and Community-based Services (HCBS) waiver program.
The HCBS waiver was established to allow states to develop group homes as alternatives to institutional care. However, the Medicaid statute did not seek to abolish institutional or ICF care. Such care must remain as an option as long as states such as Massachusetts receive federal Medicaid reimbursement for operating ICFs.
The Medicaid statute states that if a state does include ICFs in its “Medicaid State Plan,” as Massachusetts does, the state must provide that:
…all individuals wishing to make application for medical assistance under the (state) plan shall have the opportunity to do so, and that such assistance shall be furnished with reasonable promptness to all eligible individuals. [42 U.S.C. § 1396a(a)(8)]
There is nothing in the Medicaid statute that exempts states from offering an ICF as an option in response to an application for that form of medical assistance. Persons who are found to be eligible for HCBS waiver care, as Kristen was, have been found to meet the eligibility requirements for ICF-level care.
Moreover, federal Medicaid regulations state explicitly that individuals seeking care, and their families and guardians, should be “given the choice of either institutional or home and community-based services. [42 C.F.R. § 441.302(d)] (My emphasis.)
DDS official makes inaccurate claims about ICF closures
In an April 19 email to Karen and others in the case, Fuller made a number of additional statements, which we believe are inaccurate, to support the DDS position that the Wrentham Center is not open to new admissions. She stated in the email that:
As to the question of admission to the Wrentham Developmental Center, admissions to all institutional care facilities were closed with the settlement of the RICCI class action lawsuit. Many of the facilities are completely closed. The last one to close was the Fernald Center in Waltham. From the settlement agreement, DDS is to provide the least restrictive community setting options for people who are determined eligible for DDS.
In our view, this statement is largely untrue. Fuller referred in it to the Ricci v. Okin class action lawsuit, which was filed in the 1970s in Massachusetts in response to poor care and conditions in what were then referred to as “state schools” for persons with I/DD, including the Wrentham and former Fernald Centers.
The Ricci case was never “settled.” It was turned into a federal consent decree, which actually resulted in upgrades at the then existing developmental centers in the 1980s.
Moreover, the Ricci case itself didn’t result in the closures of any of the developmental centers. Fernald and a number of other developmental centers were closed as a result of policies instituted by a succession of Massachusetts governors from the 1990s onward.
Many Fernald clients were actually transferred, based on requests by their families or guardians, to the Wrentham Center, which continued to admit a handful of new clients in recent years.
Our Public Records Request
Given the concerns this case raises for us regarding the apparent lack of standard criteria for admissions to the Wrentham and Hogan Centers, we filed a Public Records Request on April 24 with both DDS and EOHHS, asking for their written policies concerning admissions to Wrentham, Hogan, and state-operated group homes in Massachusetts.
On May 7, EOHHS stated that that agency did not have any records responsive to our request. DDS stated that it needed an additional week — until May 15– to provide us with a response.
If the administration does not consider someone with Kristen’s functional limitations and medical problems a suitable candidate for the Wrentham Center, we fear it may spell the beginning of the end for ICFs in Massachusetts. Wrentham and Hogan are critically important pieces of the fabric of care for some of the most vulnerable persons in this state.
We hope our state legislators will get involved to put pressure on the administration to follow the law, and to recognize the needs and desires of Kristen, her family, and many others like them who are similarly seeking residential placements at Wrentham, Hogan, and other state-run facilities.
Update: The political and media attacks on Fernald keep coming
As we reported last week, the long-closed Fernald Developmental Center has remained a target for opponents of state-run congregate care for persons with intellectual and developmental disabilities.
We noted that on April 4, GBH News, a Boston-based National Public Radio affiliate, reported that the federal government was investigating a privacy breach involving records of former residents after Fernald was closed in 2014.
The privacy breach obviously had nothing to do with how Fernald actually functioned. But as we explained in our post, Fernald’s opponents nevertheless appear to be using the privacy issue to tarnish Fernald’s reputation.
GBH quoted an attorney with the federally funded Disability Law Center as saying that the privacy breach “challenges us to ask about how we allow institutions like Fernald to exist.”
Our concern is that opponents of state-run Intermediate Care Facilities (ICFs) for persons with intellectual disabilities in Massachusetts are using the media to help them make a case for closing those facilities. The administration, meanwhile, is continuing to let the two remaining congregate care ICFs in Massachusetts – the Wrentham Developmental Center and the Hogan Regional Center – die by attrition.
A second attack on Fernald in a week
Since our blog post ran last week, the ICF opponents and the media struck a second time against Fernald.
On April 11, The Boston Globe reported that the State Police kept unsecured records and material for criminal cases on the Fernald grounds, including evidence from homicide investigations. Again, that issue has nothing to do with how Fernald itself was managed while it operated, or with the care it provided.
Yet, both the Globe and the GBH highlighted in their reports a selected portion of Fernald’s history prior to the 1970s – a period in which Fernald and similar institutions in Massachusetts were sites of abuse and neglect.
Not only is that selective history irrelevant to the State Police and patient privacy records scandals, but both media outlets have consistently failed to mention significant and transformative improvements that were made at Fernald and those other facilities starting in the late 1970s.
The Globe, in discussing the latest “blow to the legacy of Fernald” involving the State Police records, mentioned in the story that Fernald “housed patients (my emphasis) with developmental or physical disabilities for more than a century in Waltham before closing in 2014.
“Many residents also experienced abuse at the school,” the Globe added, “including some children who were fed radioactive oatmeal as part of a science experiment.”
GBH, in its report on the privacy breach, mentioned that, “The school (Fernald) is known for troubling medical experiments conducted by MIT and Harvard, where breakfast cereal was laced with radioactive iodine.” (link in the original)
As we’ll discuss below, the radioactive oatmeal experiments took place in the 1940s and early 1950s at Fernald. They were discontinued after that time.
In its statement about the experiments at Fernald, GBH echoed a story it had published on February 27 about people who are seeking records concerning loved ones who formerly lived at Fernald. That article stated, “The Fernald,” as the school was known in the Boston area, has long been shuttered, haunted by reports that it let Harvard University and MIT perform experiments on its children, including lacing their oatmeal with radioactive iodine.”
Upgrades in the 1980s
Despite our reminders to those media outlets, neither the Globe nor GBH mentioned the upgrades in care and conditions that occurred at Fernald and at other similar facilities in Massachusetts under the supervision of then U.S. District Court Judge Joseph Tauro in the late 1970s and 1980s. After 1993, those facilities provided care that Judge Tauro deemed to be “second to none anywhere in the world.”
Far from simply “housing patients,” facilities such as Fernald, Wrentham, and Hogan were, or are, required to comply with strict federal standards under the Medicaid law for ICFs. Those standards are far more rigorous than the requirements for group homes in Massachusetts, which operate under a waiver of the standards.
A third attack on Fernald in one week
GBH’s April 4 story on the federal probe of the privacy breach was a follow-up to an initial article and photo essay by the Globe in January about the matter. Then on April 11, the same day the Globe’s State Police records story ran, GBH ran a story headlined, “Waltham residents, community members ‘enraged’ over plans for the Fernald property.”
That article addressed what the news outlet characterized as citizen outrage over a plan by the City of Waltham for reuse of 16 of the 196 acres of the Fernald campus. GBH noted that the plan would establish “memorial and universal” park areas near Trapelo Road, a “universally accessible” playground, an electric train, a mini golf course, and a spray park “that would make it the largest disability-accessible park in New England.”
The plan sounds quite reasonable to us, especially since it would be disability accessible. But GBH painted the reuse plan in largely negative terms. The media outlet said a resident told them that “she and other Waltham residents are ‘enraged’ with new plans to build a recreational park on part of the property.”
As GBH explained it, Waltham residents are apparently angry that the reuse plan didn’t sufficiently recognize Fernald’s uniquely dark history. As the resident, quoted by GBH, said, “It’s just obscene to me for them to build something that’s for amusement on a sacred ground that should be memorialized and considered more of a contemplative place to respect what’s happened in the past.” (my emphasis)
GBH then stated in the article that a former Fernald resident said “he’d like to see a museum built on the site that documents the Fernald’s complicated past.” And once again, the news outlet informed us that “The school is known for troubling medical experiments conducted by MIT and Harvard, where breakfast cereal was laced with radioactive iodine.”
It’s not clear to us that the entire City of Waltham is enraged by the memory of Fernald or even by the reuse plan. GBH stated that citizens spoke for nearly three hours at a March 27 City Council hearing on the reuse plan that was “prompted by complaints from residents.”
I listened to several portions of the hearing, which is posted online. Some residents during the hearing did appear to refer in negative terms to Fernald’s history prior to the 1970s.
But there were also concerns expressed during the hearing about the impact of the reuse plan on wetlands, and that the recreational activities would be sited too close to their homes on Trapelo Road. Not everyone was outraged over Fernald’s past. As GBH acknowledged, a few residents even expressed support for the plan.
The radioactive oatmeal story
While the improvements overseen by Judge Tauro at Fernald are never mentioned by the media, the radioactive oatmeal scandal is mentioned in virtually every media account written about the former center.
Since February, GBH has mentioned the oatmeal story in at least three stories. The Globe referred to the oatmeal story in its State Police records story and in the January article and photo essay about the privacy breach involving patient records.
The January 10 Globe article described Fernald as follows:
The school was founded in 1848, and its name has become synonymous with American institutional mistreatment of disabled children. Patients were malnourished, abused, and segregated from society well into adulthood. Some were also made unwitting participants in medical experiments, such as the “Science Club,” in which scientists from MIT and Harvard fed children radioactive isotopes in their oatmeal from 1946 to 1953. Quaker Oats was the sponsor.
As usual, no mention was made in that article about Fernald’s history after the 1970s.
Of course, a series of troubling experiments in which radioactive oatmeal was served to Fernald residents did take place in the 1940s and early 1950s. These experiments apparently came to light in 1994.
But while these experiments were shameful, exactly what the State Police records and privacy scandals on the Fernald grounds have to do with those experiments, which took place some 65 to 75 years earlier, is more than a little unclear.
We, along with proponents of the Fernald Center, have, on a number of occasions, contacted both GBH and the Globe to try to correct the record, and to urge them to consider the entire history of Fernald in their coverage.
We have also contacted key members of the state Legislature to let them know that we think Fernald’s history is far richer than what is being reported by the media.
As noted, we think the continuing media coverage of Fernald is an important issue because of the implications this kind of reporting may have on the Wrentham and Hogan Centers and on the future of state-run care in general for some of the most vulnerable people in our society.
We fully support transparency with regard to the care of persons with intellectual and developmental disabilities, and we support efforts to bring the history of that care to light, warts and all. But that history should be told in its entirety, and should not be selectively reported in order to further political agendas.
Fernald opponents appear to be using privacy breach to tarnish the reputations of remaining ICFs in the state
The Fernald Developmental Center has been closed for a decade, but it remains a political lightning rod for opponents of state-run care for persons with intellectual and developmental disabilities in Massachusetts.
The latest organization to attack Fernald is the federally funded Disability Law Center (DLC), which appears to be using a recently discovered breach of the privacy of former Fernald residents to further tarnish the reputations of Fernald and two remaining Intermediate Care Facilities (ICFs) in the state.
The Boston-based DLC is a legal rights advocacy organization that has long lobbied for the closure of congregate care settings and for the expansion of the state’s network of privatized group homes.
GBH News, a Boston-based National Public Radio affiliate, reported last week that the DLC has filed a complaint with the federal Office of Civil Rights (OCR) alleging a privacy breach involving records of former Fernald residents. The DLC complaint is based on the publication of photos in January by The Boston Globe showing what appear to be large numbers of those records, which had been dumped on the floors of now-abandoned buildings on the campus.
The OCR, which is under the U.S. Department of Health and Human Services, has opened an investigation of the alleged records breach based on the DLC’s complaint.
While we strongly support the OCR’s investigation, it is a statement made by an attorney with the DLC concerning the alleged breach that caught our attention. The attorney is quoted in GBH’s story as saying the following:
Why do these things (privacy breaches) happen to people with intellectual and developmental disabilities, and don’t happen to able bodied people? It challenges us to ask about how we allow institutions like Fernald to exist to begin with, and how we haven’t reckoned with the history of those institutions. (my emphasis)
Leaving aside the fact that privacy breaches can and do happen to both disabled and non-disabled people, we would agree that the breach in patient privacy at Fernald implies a major managerial failure on the part of the state, and we think the administration should take responsibility for it.
But what does a privacy breach have to do with whether Fernald should have existed, and why should the blame for that particular breach be placed on the people who ran and worked at Fernald? It is the state administrators who were in charge of closing Fernald and disposing of the property who should have seen to the proper handling and storage of the residents’ records.
Moreover, in saying the privacy breach “challenges us to ask about how we allow institutions like Fernald to exist,” the DLC attorney appears to be referring to the Wrentham Developmental Center and the Hogan Regional Center, the only two institutions like Fernald that still do exist in Massachusetts. It thus appears that the DLC is using the records breach involving Fernald to tarnish the reputations of Wrentham and Hogan, perhaps in order to push for their closure.
We hope neither the Healey administration or the Legislature falls for this. It’s a red herring.
As we have frequently reported, the administration is effectively allowing state-run residential services for people with developmental disabilities in Massachusetts to die by attrition. This will spell disaster for the care of those people.
The Healey administration and the DLC know full well that many privatized group homes have become the new warehouses of abuse and neglect in Massachusetts. The Department of Developmental Services (DDS) is unable to adequately oversee the system, and is obsessed, as the Globe has reported, with retaliating against families and guardians who dare to complain about poor conditions in corporate provider-run group homes and day programs.
We would note that the DLC, over the years, has turned down a number of requests for legal representation by individuals we advocate for, saying the DLC lacks resources. Yet the DLC is apparently continuing to use its limited resources to push for the closure of two state-run facilities that provide a critical backstop for care in the DDS system, and that are subject to stricter oversight and that provide care that meets stricter federal standards than the standards that apply to group homes.
Consistent focus on the early history of Fernald
It is also apparent, based on the DLC’s complaint and GBH’s coverage of it, that both organizations are interested only in discussing the darkest periods of Fernald’s history prior to the 1980s. There is no mention by either the DLC in its complaint, or by GBH, of the significant improvements at Fernald and other similar institutions in Massachusetts that were made as a result of the intervention of the late U.S. District Court Judge Joseph L. Tauro, starting in the 1970s.
What the DLC complaint does say is that the failure to secure medical records after Fernald’s closure:
…places additional barriers before…historians documenting the practices which took place at this site (Fernald) over decades. This includes promotion of eugenics, squalid living conditions, physical abuse, and as noted in the Globe article, the ‘Science Club’ experiments of feeding children radioactive isotopes in their oatmeal over a seven year period. (my emphasis)
Similarly, GBH, in its article on the DLC’s complaint, stated:
The Fernald, as it was widely known, is home to a dark history of abuse, including reports of research on children by Harvard and MIT that laced breakfast cereal with radioactive iodine. (link in the original)
But these terrible episodes of Fernald’s history had largely ended by the 1960s – a half century before Fernald was closed over the objections of the families of many of its remaining residents in 2014.
As we have pointed out before, the man for whom the institution was later named—Walter E. Fernald—was initially an active proponent of eugenics laws that were being adopted in the late 19th and early 20th centuries in the U.S. But by the 1920s, even Walter Fernald had come to reject the principles of eugenics, and “became a supporter of community placement…” for persons with developmental disabilities, according to the Encyclopedia Britannica.
The radiation experiments on children took place from the 1940s through 1961, according to the GBH link above.
This is not to suggest that these abuses and immoral racial theories that involved Fernald should not be studied or publicized in order to warn us not to repeat that history. But to make those events the sole focus of any historical account of Fernald raises questions about the political agenda of those engaging in it.
Judge Tauro noted the positive transformation that Fernald and other similar facilities had undergone when he disengaged in 1993 from his oversight of Ricci v. Okin, the landmark consent decree case that brought about those improvements.
Tauro wrote that the improvements had “taken people with mental retardation from the snake pit, human warehouse environment of two decades ago, to the point where Massachusetts now has a system of care and habilitation that is probably second to none anywhere in the world.”
Proposed state commission also appears to have a bias
As we have reported, a state commission created by the Legislature in 2022 to study the history of Fernald and other similar facilities in Massachusetts also appears likely to have a similar bias against today’s congregate care models, and a similar fixation on Fernald’s early history.
In February, after GBH published an article discussing the commission uncritically, we informed the news station of our concern about the commission’s potential bias and its proponents’ apparent disinterest in Judge Tauro’s role in improving Fernald and the other facilities. Unfortunately, a noted above, our perspective was not recognized in GBH’s subsequent coverage of the alleged privacy breach.
We certainly hope it isn’t the case that this administration is ready to abandon state-run residential care and that it plans to cite the Fernald privacy breach as a pretext for doing so. So far, we haven’t been able to get the administration to make any sort of public statement about its intentions with regard to either the Wrentham or Hogan Centers, or about the commonwealth’s similarly declining network of state-run group homes.
Until the administration does signal its intentions in this regard, we’re left to read the tea leaves. And as usual, it is the former Fernald Center and how it is still portrayed by its long-time adversaries long after its death that appear to provide those possible clues.
Mother of autistic child criticizes NIH and medical journal article that liken efforts to prevent autism in children to eugenics
Is it really a form of eugenics to advise pregnant mothers to avoid taking hormones such as testosterone that may cause their babies to develop neurological disorders such as severe or profound autism?
We don’t think having a concern about the effect of testosterone on fetal development is in any way akin to eugenics. But that appears to be the position of the National Institutes of Health (NIH), which is considering removing a goal of reducing disability from its mission.
In an essay last month, Amy Lutz, vice president of the National Council on Severe Autism (NCSA), criticized both the NIH and an article in the research journal Social Science and Medicine – Qualitative Research in Health for promoting the eugenics charge.
We support the mission of Lutz’s organization, which advocates for increased services and research to benefit the often-neglected population of people with severe and profound autism.
The Social Science journal article concludes that health care providers who advise pregnant transgender people to stop taking testosterone are being improperly “fetal-focused” and “eugenicist.”
A key statement in the journal article is the following:
The desire to maximize the ‘fitness’ of offspring, and guard against development of conditions or human characteristics considered ‘unhealthy’ or less than ideal, may reflect troubling eugenicist and biomedical moralist underpinnings in ways that further harm already socially-marginalized people.
Lutz also noted that NIH recently announced that it was considering removing the goal of reducing disability from its mission statement. This was being done, Lutz said, at the recommendation of an NIH advisory committee that “blasted the idea that disabled people need to be ‘fixed,’ as ‘ableist.’”
We have written before about the Lutz’s organization’s efforts to expose and rebut a groundless but growing ideology that no matter how profound a person’s developmental disability might be, they have an unlimited potential for achievement in mainstream society, and that autism is not even a disability.
We have seen that this ideology results in a reduction in services for developmentally disabled people and a reduction in our society’s concern for the wellbeing of disabled children and adults, and for the wellbeing of their families.
Does that “make me a eugenicist?”
Lutz is the mother of a profoundly autistic son, Jonah, 25. She maintained that, “Not only would I cure him if it were possible, but if I could eradicate profound autism in future generations, I would without hesitation. Now, considering the tenor of these online debates, I was forced to consider: did that make me a eugenicist?”
The Social Science and Medicine article specifically criticizes advice given by many health care providers to transgender persons who are trying to conceive children to discontinue the use of the male hormone testosterone.
The journal article authors note that for many trans people, testosterone treatment results in improvement in their mental health, including reductions in depression and anxiety. At the same time, the authors concede that concerns have been raised that babies born to trans persons taking testosterone could develop “neuropsychiatric disorders” such as Autism Spectrum Disorder (ASD) and suffer other medical problems.
Concern about testosterone use during pregnancy is ‘fetal-focused’
The Science and Medicine journal authors appear to agree with some health care providers that there has been a lack of research to either rule in or rule out testosterone use by trans persons as a possible cause of fetal abnormalities. Nevertheless, the authors contend that those concerns, whether they are correct or not, are improperly “fetal-focused.”
The journal article goes on to state:
Ultimately, we argue that in the context of lacking and uncertain medical evidence (about testosterone use by pregnant trans persons)… both patients and providers tend to pursue precautionary, offspring-focused treatment approaches. These approaches reinscribe binarized notions of sex, resulting in social control in their attempts to safeguard against non-normative potential future outcomes for offspring. (My emphasis.)
These offspring-focused risk-avoidance strategies and approaches are, we argue, part of the gendered precautionary labor of pregnancy and pregnancy care itself, and not without potentially-harmful consequences for trans people and society more broadly.
Thus, the journal article authors appear to imply that the potential loss of personal wellbeing experienced by a pregnant trans person in having to stop taking testosterone is a more serious matter than the possibility that continuing to take the male hormone could medically or cognitively harm their fetus.
Lutz maintains that her son requires round-the-clock care. Without prompting, he would never brush his teeth, shower, put on a coat, or take the medicine that controls his seizures and minimizes his aggressive behavior, she wrote. That behavior required him to be hospitalized for almost a year when he was only nine years old.
“He (Jonah) has no safety awareness,” Lutz added. She and her husband have code locks on all the exterior doors to prevent Jonah from wandering—”a dangerous behavior exhibited by more than half of autistic children, and one of the leading causes of premature death in this population.”
Lutz said that as the vice president of the NCSA, she constantly hears from parents who have been forced to quit their jobs to care for children with profound autism, and about profoundly autistic adults “warehoused in emergency rooms…If NIH removes the goal of reducing disability from their mission statement, they will fail every single one of these families, and push an already marginalized population so far out of public discourse that they—and their intensive, lifelong needs—will become virtually invisible.”
Yet, according to the authors of the Social Science article, those concerns by those families are “imbued with normative” and “fetal-focused” judgments, and “reflect troubling eugenicist” views.
For Lutz, the argument that disability is neutral “may sound progressive and empowering, but it betrays complete ignorance of what severe intellectual and developmental disability looks like, or how it impacts affected individuals and their families.”
Disability advocates such as the authors of the Social Science article are trying to “aggressively shut down incongruent narratives with accusations of ‘eugenics’ and ‘ableism,’” Lutz maintains.
We would agree with Lutz. In our view, the Social Science authors and the NIH should realize that if they are truly concerned about the emotional wellbeing of transgender mothers, they should consider the impact on their lives of having to care for a child that grows into an adult with severe intellectual disability or autism.
Family faces Catch-22 from DDS in trying to get residential services in Massachusetts for their daughter
When Lara Dionne and her husband Martin attempted to bring their intellectually disabled daughter Keridwen from Maine to Massachusetts, they didn’t realize they would face a Catch-22-style series of bureaucratic rules and roadblocks from the Massachusetts Department of Developmental Services (DDS).
Keridwen has severe behavioral problems that require that she be placed in a secure setting, so the Dionnes requested a placement for her at the Hogan Regional Center in Massachusetts. She is currently living in an institutional facility in Maine.
However, DDS responded that it wouldn’t even consider whether Keridwen was eligible either for care at Hogan or for any other services until she was living in Massachusetts. DDS officials told the Dionnes they would have to bring Keridwen to Massachusetts in order for the eligibility determination process even to begin.
But, as we have reported, that eligibility determination process can take up to a year or more to complete. As a result, Keridwen would not have any services during that time, Lara said, and Keridwen and those around her would be at risk of harm due to her frequently violent behavior.
Yet, if the Dionnes were to leave Keridwen in the institution in Maine, the eligibility process for services for her in Massachusetts would never start.
“That scenario would effectively bar her (Keridwen) from ever moving to Massachusetts,” the Dionnes asserted in a statement filed with a DDS hearing officer who is considering their appeal to allow their daughter to be processed for eligibility in Massachusetts while she stays in the facility in Maine.
On top of all of this, as we have also reported, it is nearly impossible for adults with intellectual and developmental disabilities (I/DD), much less a 19-year-old such as Keridwen, to gain admission to either the Hogan Center or the Wrentham Developmental Center. That is because the doors to these two Intermediate Care Facilities (ICFs) have essentially been closed to individuals seeking admission.
The Dionnes say they are additionally facing pushback from the Salem School District, which funds care for district residents with intellectual and developmental disabilities who are under 22 years of age.
Lara and Martin, who moved to Salem from Maine last fall, are struggling to figure out how to get Keridwen moved closer to them safely. They said that because DDS won’t start the eligibility process, they also have no case management services for her in Massachusetts.
Massachusetts eligibility process takes a year or more
Lara said that when she first inquired about the Hogan Center, she was told she would need to apply first to DDS for eligibility for services. She said she was also told, at the time, that the eligibility process was taking 11 months.
Under DDS regulations, however, the Department must determine eligibility for supports and services within 60 days. But internal departmental emails, which we received from DDS, indicate that hundreds of individuals are being forced to wait for up to a year or more to be ruled eligible for those services.
The emails confirmed that DDS has been dealing with a backlog of eligibility applications due to a shortage of psychologists who are needed to make eligibility determinations on an individual basis.
DDS treated Keridwen’s application under adult regulations
DDS regulations actually allow for persons under 22 to be considered to be living in Massachusetts if one or both of their parents are living in this state. That is the case with the Dionnes, who both moved to Massachusetts from Maine last November.
But for reasons that have not been explained to them, the Dionnes said DDS is applying an adult eligibility regulation to Keridwen even though she is 19. The adult regulation states that the applicant for eligibility must reside in Massachusetts, regardless of where their parent lives.
The Dionnes, however, maintain that even under the adult regulations, Keridwen can legally be said to reside in Massachusetts as well as in Maine.
Since January 2023, Lara said, she has informed DDS that the family’s intention is for Keridwen to join the family in Massachusetts as soon as a suitable facility can be found for her. Keridwen stays with her parents in Massachusetts at least one weekend per month, and she has a bedroom in their home.
No response to request for a secure environment at Hogan
In early 2023, the Dionnes first inquired of DDS about applying for eligibility for services for Keridwen, and about “transitioning services between Maine and Massachusetts.”
In response, Erin Krol, the DDS Northeast regional eligibility director, stated on February 6, 2023, that, “Unfortunately, we do not have any means to transfer a person from one state to another.”
Krol added that, “an individual must apply for DDS eligibility in Massachusetts and go through the Eligibility process.” That process, Krol said, “requires the applicant to be domiciled in the Commonwealth of Massachusetts.” Only then, she said, could the Dionnes submit documentation “to proceed with the application.”
Lara responded to Krol with an email, saying, “We are not asking to jump the Massachusetts queue for services. We know there are waitlists. We are asking to get in those queues to transition her services safely.” She explained that her daughter has a history of behavioral issues, “including property damage and assault causing lasting bodily harm. I am not capable of caring for her alone.”
In June 2023, Lara emailed Kelly Lawless, DDS’s Northeast regional director, to express her and Martin’s desire for a placement for Keridwen at Hogan. She noted that only an ICF, which meets strict federal standards for staffing and care, could ensure her safety.
The following month, Lara wrote again, saying, “We hope that there is a children’s residential program appropriate to her (Keridwen’s) level of need in Massachusetts, but we have some concerns there. She is in an actual institutional setting currently.”
Lara noted in that message that, “we cannot bring her down here safely without placement in a treatment facility (and an educational facility) that has training in safe restraint, multiple staff on hand to execute such restraint, a medical team to address her psychiatric medications in a timely manner to respond to behavioral crisis, a secured physical environment which prevents access to hazards, and 24/7 staffing to cover any elopement attempts at night.”
In response, Krol suggested that the Dionnes “focus on getting (Keridwen) enrolled and placed appropriately in Massachusetts through the school district and then work with her team at Salem Public Schools on transitional planning for when she is 22 years old.” Lara said neither Krol nor Lawless responded to Lara’s statements about the need for a secure, ICF-level placement for her daughter.
Eligibility denied
The Dionnes applied for eligibility for DDS services in Massachusetts for Keridwen in November 2023. Only two weeks later, in December, DDS informed them that Keridwen had been found ineligible for services because she was “not domiciled in Massachusetts as per (the adult services eligibility regulation).”
The Dionnes appealed the eligibility denial, and had a DDS-sponsored “fair hearing” on March 13. Closing arguments in the appeal are due in late April. But the hearing officer is a DDS official, and the Dionnes said that as a result, they are not expecting that they will win their case.
DDS denial rests on definition of ‘reside’
As noted, the basis for the quick eligibility denial was the Department’s adult domicile requirement in its regulations (115 CMR 6.04). In an email in response to the denial, Lara contended to Lawless that “Domicile requirements for 5-22 year-olds are governed by 115 CMR 6.06 (the children’s eligibility standard under DDS regulations).”
In a subsequent statement filed with their appeal, the Dionnes maintained that, “No explanation is provided for why her (Keridwen’s) eligibility was not evaluated on the basis of children’s supports. Nor does it indicate what aspect of the domicile requirements were unmet.”
The Dionnes argued that even under the adult regulations, Keridwen could be considered to reside in Massachusetts. As noted in Black’s Law Dictionary, they stated, “A person domiciled in one state may, for temporary reasons such as health, reside for one or more years in some other place deemed more favorable.”
The Dionnes noted that the DDS regulations do not state that the person must “reside solely in Massachusetts,” nor do they specify any limits on how much of the time they must reside here.
“To deny eligibility for DDS services based on a more restricted interpretation of ‘reside’ would create an untenable paradox,” the Dionnes stated. “We cannot safely relocate Keridwen to Massachusetts without continuity of care. And yet we would not be able to arrange those services without her first relocating to Massachusetts. That scenario would effectively bar her from ever moving to Massachusetts.”
No response from the administration
Lara said that in addition to making their case to DDS, she and her husband have contacted the Executive Offices of Health and Human Services and the Governor’s Office of Constituent Services, and sent them “multiple calls, emails, and a letter with supporting documentation.” She said they have not received a response from either office.
The Massachusetts Attorney General’s Civil Rights Division, which the Dionnes had also contacted, did respond with a letter stating the Division was “not able to assist in resolution of this matter.”
Unfortunately, the direction this case has taken is not surprising. DDS has declined to accommodate this family, which is clearly in need of the Department’s help in a difficult situation. The Department has instead placed a priority on its policy of keeping the doors closed to the Hogan Developmental Center, a critical piece of the state’s infrastructure for persons with intellectual and developmental disabilities.
The Department has also interpreted its rules concerning domicile in Massachusetts in an unfavorable way with regard to the interest of this family. It applied an adult standard, without explaining its reasoning for that. Higher-ups in the administration, including the governor’s office, have not responded to the family.
The Dionnes said the Salem School District has similarly pushed back against their wish for residential accommodations for their daughter. In our view, the District is most likely doing this for budgetary reasons. Neither governmental entity – DDS nor the Salem Schools – appear to be acting on behalf of their most vulnerable constituents who need their help.
This is yet another reason why we are asking the co-chairs of the Legislature’s Children, Families, and Persons with Disabilities Committee to intervene with DDS, in particular, on behalf of some of the most vulnerable members of our society. We hope we will receive a response from those co-chairs before it is too late for people like Keridwen and her family.
State legislators could help change the culture in DDS. Will they?
More than a month ago, we brought a case involving the apparent neglect of a resident of a provider-run group home and the intimidation of his family to the attention of the co-chairs of the Legislature’s Children, Families, and Persons with Disabilities Committee.
Then on March 5, I forwarded a follow-up post about the case to the committee co-chairs, Senator Robyn Kennedy and Representative Jay Livingstone.
We think the case illustrates a disturbing and ongoing state of dysfunction in the state’s system of care of persons with intellectual and developmental disabilities (I/DD). It seems that the Department of Developmental Services (DDS) is doing little or nothing to change a culture in the system that appears to foster this level of neglect and intimidation.
As our posts reported, Rachel Surner informed the upper management of her son’s corporate provider-run group home in June 2022 of an incident in which the staff neglected to give her son Ian his portable urinal. Ian, 31, has spastic quadriplegia, a condition that has left him with the limited ability to move only his arms.
Having received distress texts on her phone from her son, Rachel had to go to the home herself at 6:45 in the morning to retrieve his urinal from the floor next to his bed.
Then in January of this year, the same thing happened again when the same staff member again allegedly neglected to give Ian his urinal. The response of the provider, the Justice Resource Institute (JRI), however, was to blame Rachel for allegedly being “disruptive” in the home, and to impose severe restrictions on her visits to her son.
DDS stated that Rachel and her husband would either have to comply with those restrictions or remove Ian from the home.
Rachel had complained about numerous other problems in the home as well, including a failure to regularly shower or toilet Ian, and a failure to involve him in community activities.
On February 12, I talked to a member of Senator Kennedy’s staff at a meeting she held with constituents in my hometown of Berlin, MA, and gave her information about Ian’s case and that of another mother whose son was also severely neglected in a provider-run group home.
In that second case, the son had suffered extreme dental decay, weight loss, removal of prescribed medications, and unexplained injuries. The aide said she would bring the cases to Senator Kennedy’s attention.
Not having heard anything more by the beginning of this month, I stated in my March 5 follow-up message to both Kennedy and Livingstone and their staffs that we would be happy to arrange for our members to provide them with further information about the ongoing problem of abuse and intimidation in the DDS system.
Even The Boston Globe has written about this culture, noting earlier this year that when parents of children with autism have complained about abuse and neglect in DDS-funded group homes, they have been labeled as “too demanding.” And a number of parents who spoke to the newspaper requested anonymity because “they were afraid that state officials or providers would retaliate against them.”
Obligation to change the DDS culture and system
We think legislators have an obligation to help change a culture within DDS that appears to perpetuate poor care and intimidation of families in the provider-run group home system. As co-chairs of the Children and Families Committee, Kennedy and Livingstone are in a position to exert pressure on DDS to change that culture.
Last fall, we first met with both Senator Kennedy and Representative Livingstone on Zoom to make a case for the preservation of state-run residential services. In our view, state-run services are more accountable to both families and taxpayers than are corporate provider-run services.
Levels of abuse and neglect in the Wrentham and Hogan facilities are significantly lower than in the provider-run group home system, based on a review of state data that we undertook.
On a per-client basis, state-operated group homes were well below average in terms of both substantiated allegations of abuse and criminal referrals between Fiscal 2010 and 2019. Also, we found that the state-run Wrentham and Hogan Intermediate Care facilities were at or near the bottom of the list of total providers in those measures.
Yet, the Wrentham and Hogan Centers and the state-run group homes are ultimately facing closure because a succession of administrations has largely closed their doors to new admissions.
Last fall, Senator Kennedy said she would help us arrange a meeting with Governor Healey in which we would raise these concerns. We urge people to email Kennedy’s and Livingstone’s offices, and forward a link to this blog post.
You can email them at Robyn.Kennedy@masenate.gov and Jay.Livingstone@mahouse.gov.
Remind them that it is time to change the culture in DDS and to take concrete steps, including setting up a meeting with the governor, to preserve state-run services in the DDS system.
Thanks!
Mother says neglect and intimidation continued at her son’s group home
More than a year and a half ago, Rachel Surner informed the upper management of her son’s group home in Ashland of a disturbing incident in which the staff neglected to give her son, Ian Murawski, his portable urinal.
Rachel had to come to the house herself at 6:45 in the morning in June 2022 to retrieve the urinal, which was on the floor next to Ian’s bed. She said she was met at the door with resistance and intimidation by a staff member on duty.
Ian, 31, has spastic quadriplegia, a condition that has left him with the limited ability to move only his arms. Despite that, Ian, who has an intellectual disability, is an engaging young man with a major musical singing talent.
Rachel also informed the Department of Developmental Services (DDS) about the June 2022 incident, and a range of other problems in the group home, which is run by the Justice Resource Institute (JRI), a corporate DDS provider. But nothing was ever done to improve the situation, she said.
Following an almost identical incident in January of this year in which the same staff member again neglected to give Ian his urinal, Rachel said JRI’s response was to blame her for allegedly being “disruptive” in the home.
JRI then imposed severe restrictions on her visits to her son, and DDS stated that she and her husband would either have to comply with those restrictions or remove Ian from the home.
Rachel and her family chose the latter course. They took Ian home last month to live with them.
They are seeking another placement, and are interested in the Wrentham Developmental Center or possibly a state-operated group home. But, Rachel said, DDS has provided few answers to their questions about those options.
As we argue below, we believe that in issuing the visitation restrictions, JRI violated DDS regulations ensuring a right to visitation. Also, we think DDS violated its transfer regulations that prevent the termination of residential services to individuals without due notice and due process.
This is one of many cases in which providers and DDS appear to have placed the blame on family members for being disruptive or overly demanding when they have attempted to advocate for their loved ones in group home settings. (See here, here, and here.) In all of these cases, DDS has appeared to side with provider staff against the families when those families are simply complaining about substandard care.
‘Passive-aggressive torture”
Rachel and her husband, who deny having ever caused a disturbance in the home, said the latest incident in January occurred after her son had called her repeatedly, screaming and “in crisis.”
Ian, who is high-functioning despite his disability, takes medication for extreme anxiety and depression, which can reach levels high enough to cause psychosis, Rachel said. However, the staff didn’t give the medication to Ian regularly because they didn’t pay enough attention to him to recognize his symptoms of anxiety, she said.
According to a DDS complaint intake letter about the January 21 incident, Rachel went to the house from her home in Holliston at 11:30 p.m. after being unable to reach the staff by phone. A JRI attendant on call, whom she also had contacted, had told her that Ian was asleep. Rachel said she knew this wasn’t the case as Ian was still calling and texting her in distress.
When she entered the house, she found that Ian was awake in his bed, which had been left in an upright position. He had no remote controls for adjusting the bed, no urinal, no water, and the overhead light had been left on. Without access to the remote controls, there was no way Ian could adjust his bed or get to sleep.
According to the intake letter, a staff member, meanwhile, was lying under covers with a pillow on a couch in the living room, and was speaking on a phone in a foreign language. When Rachel asked repeatedly where the remote controls were, the staff member refused to answer and said he was on a call. At that time, Rachel pulled her phone out of her back pocket to call her daughter, and the staff person then lunged at her to grab it from her, the intake letter stated.
This was the same staff member, according to Rachel, who had neglected in the previous incident in June 2022 to give Ian his urinal. The January 2024 intake letter quoted Rachel as referring to the failure to give Ian his remote controls and urinal as “a passive-aggressive form of torture.”
The latest incident is under investigation by the Disabled Persons Protection Commission (DPPC).
June 2022 incident
As we reported last April, Ian repeatedly texted Rachel early one morning in June 2022 from the group home that he needed to urinate, but couldn’t locate his portable urinal.
Rachel said she tried to call the house, but the phone was off the hook; so at 6:45 a.m. on a Sunday morning, she drove there. As she waited for someone to answer the door, she could hear Ian crying for help.
Rachel said the same staff member, who later neglected to provide Ian with his urinal and remote controls in January of this year, came to the front door, but refused at first to let her in. She went past him into the house, and went to her son’s room where she saw that his urinal, which was supposed to be on his bedside table, was on the floor.
Rachel said that when she then tried to leave the room to give Ian privacy, the staff member initially blocked the door to the bedroom and wouldn’t move to let her out. He later moved away slightly, but she felt threatened and intimidated by his actions.
She said she later asked the staff member why he didn’t respond to Ian’s plea for help, to which he replied that Ian “’never told us he needed help.’” She said she replied to the staff member that she could hear Ian’s cries for help while she was standing at front door.
Problems not corrected
Rachel said neither JRI nor DDS made efforts to correct problems in the group home, such as the urinal incidents, that she brought to their attention. One other example of that was her discovery in July of 2023, after bringing Ian home from a musical gig at a restaurant in Ashland, that overnight staff in the home appeared to be asleep in the living room when they arrived. As noted above, she said that issue continued through this past January.
Other ongoing problems have included:
Hygiene neglect
Rachel said Ian went for days with no shower or toileting in the group home. He also went for days without having his teeth brushed. His bed linens filthy, she said, and he was often dressed in same clothing as the day before. His finger and toenails were often unclipped, and he was often not shaved.
Lack of socialization, activities, and community involvement
Rachel contends the staff rarely took Ian out of the house on community outings. She said this was due to the staff’s lack of involvement in general with him. She noted that Ian needed far more care than the other clients in the home who are all able-bodied.
Visitation restrictions violated DDS regulations
Rachel said that after the incident on January 21 of this year, JRI’s response was to issue visitation restrictions against her, which both she and a JRI program director were supposed to sign.
A copy of the unsigned and undated visitation restrictions contains the introductory statement that, “Inappropriate and disruptive behavior creating an environment detrimental to program services have occurred during visits of Rachel Surner to (the group home).”
Rachel maintains that statement is completely untrue. She maintains that neither she nor any other members of her family were ever disruptive in the home.
Rachel was then supposed to agree to the following restrictions:
- Visits may occur no more than once per day for a maximum of one hour per visit.
- No video recording of staff or other individuals may take place during the visit. (Rachel maintains she never recorded staff, but live videotaped her visits so family members could be witnesses to interactions in the home.)
- Drop-offs without entering the home or property must also be scheduled in advance with JRI management and are limited to 10 minutes.
- Parking on the street outside the property is prohibited except during agreed-upon visits.
- JRI may deny plans for any visit if it is not deemed necessary or it is detrimental to the program.
- JRI staff have the right to terminate a visit at any time. I (Rachel) agree to leave peacefully when requested or required to do so.
Rachel said the DDS assistant area director stated to her that she would have to agree to the restrictions in order for Ian to continue to live in the group home.
In our view, JRI, in issuing the visitation restrictions, was acting in violation of DDS regulations, which permit visitation by a guardian “to the maximum extent possible.” According to the regulations, “Reasonable restrictions” may be placed on the visits “to avoid serious disruptions in the normal functioning of the provider.”
Given that Rachel denies that her family ever caused any disruptions, we think DDS should have given the Surners a chance to rebut the allegation. That didn’t happen.
We also think DDS violated the Department’s transfer regulations, which prohibit the Department from terminating a residential placement without giving 45 days’ notice, specifying an alternative location and obtaining the guardian’s consent to it.
Desire for a new placement
Rachel said that since Ian’s discharge from the group home, he is not currently receiving any services from the Department. She said that while DDS did provide her with a list of other group homes, the Department has not answered many of her questions about the list.
This case is one of many demonstrating that the DDS-funded provider-run residential system has become dysfunctional. Problems identified by family members are not corrected, but the family members themselves often become the focus of blame.
DDS has consistently also blamed these problems on staffing shortages. But that doesn’t explain why the Department apparently didn’t act in this case to ensure that overnight staff were not sleeping on the job, or that the staff treated Ian with dignity and respect. Repeated failures to provide a portable urinal to a person with quadriplegia is inexcusable, and is rightly being investigated as abuse by DPPC.
Inadequate staffing also doesn’t explain why the Department would agree to an excessively restrictive visitation policy against the family, or why the Department didn’t seek Rachel’s response to the charge that she was being disruptive in the home.
DDS needs to reexamine and change its culture. In our view, this is a key test for the Healey administration.
Has the state been using hundreds of millions of taxpayer dollars in a reserve fund as promised to boost direct-care wages?
The state has appropriated more than $400 million in taxpayer funds to a human services provider reserve fund over the past two years, with at least three quarters of that amount supposed to be used to raise wages of direct-care staff of human services providers in Massachusetts.
Low wages have caused a continuing staffing shortage and worsening care in corporate provider-run group homes funded by the Department of Developmental Services (DDS).
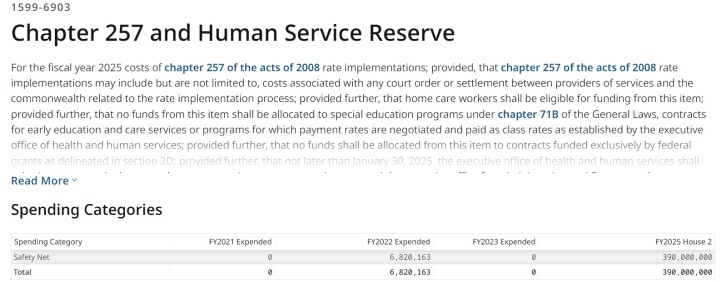
Governor Healey is now pledging an additional $390 million to the “Chapter 257 Human Services Reserve” line item in the coming Fiscal Year 2025 budget, bringing the total appropriations to nearly $800 million. Chapter 257 was a law passed in 2008 that was intended to biennially set and increase state payment rates to human services providers.
But there seems to be little or no available information thus far as to:
- The amount of money in the reserve fund that has actually been spent to date to boost direct-care wages;
- How the administration or Legislature are able to track whether providers are raising those wages.
The reserve line item has included language in the FY ’23 and ’24 budgets stating that “any human service provider receiving revenue under said Chapter 257 shall use not less than 75 percent of received funds for compensation for their direct-care, front-line and medical and clinical staff.” However, the line-item language does not explain how that requirement would be carried out or enforced.
An administration spokesperson told us that that the governor’s proposed $390 million appropriation to the provider reserve fund in FY ’25 “is based on a model that supports wages no lower than $20/hour.”
One provider executive told us their agency was paying direct-care workers $17.50 an hour. So, presumably, the administration expects that that provider’s workers will receive at least a $2.50 per hour increase in their wages.
But whether those wage increases will actually happen is unclear. Similar promises in the past haven’t been met.
Funding rates for provider-run group home and day programs are set by regulation, after a public hearing process. Those rates are calculated based on what appear to be “benchmarked” expenses for wages and non-salaried costs. It isn’t clear, however, that the providers are required to pay those benchmarked wages.
What does seem to happen regularly is that the provider executives are paid higher and higher salaries and other compensation, while direct-care worker wages stay relatively stagnant.
Compare, for instance, the average direct-care salary in Massachusetts in FY ’22 of $43,260 (see below) with the total compensation that year to David Jordan, president of the Seven Hills Foundation, a DDS provider, of $1.2 million, and to his wife Kathleen Jordan, executive vice president and CEO, of $455,351.
Inspector general and state auditor had similar oversight concerns about payment of wages
In 2022, the Massachusetts Inspector General’s Office stated it had investigated complaints that state Executive Office of Health and Human Services (EOHHS) providers had misused $139 million in COVID pandemic relief funds that were supposed to be spent on direct-care staffing and other activities. Instead, providers allegedly spent the funds on executive salaries.
The IG stated that EOHHS did not fully implement its recommendations to develop detailed provider expenditure reports regarding state funding intended to be spent on staffing. The IG also stated that EOHHS failed to provide guidance to providers on reporting those expenditures.
In 2019, the state auditor found that major increases in funding to the human services providers Under Chapter 257 had led to surplus revenues for the providers, but had resulted in minimal increases in wages to direct-care workers.
We are asking both the IG and State Auditor to investigate the management and oversight of the reserve fund.
No clear oversight or tracking of direct-care wages by the state
It remains unclear how the state verifies or tracks the amount that human services providers pay in wages to their direct-care and other frontline workers. We asked this question of both administration officials and legislators, and have received no answer to it.
Oversight processes used by the state involving the provider reserve fund raise a number of similar questions.
For instance, in the FY ’23 and FY ’24 state budgets, the provider reserve fund language required EOHHS to provide a report to the Legislature’s House and Senate Ways and Means Committees on “ongoing and proposed initiatives” to increase direct-care wages. Those reports were required to be submitted in March 2023 and April 2024 respectively.
However, the March 2023 report, which COFAR obtained under a Public Records request, did not appear to provide that information. There was no mention in the report of any specific initiatives to raise direct-care wages, or even of the amount of funding appropriated under the provider reserve line item in that fiscal year.
The requirement that providers spend 75% of their reserve account funding on direct-care wages wasn’t mentioned in the March 2023 EOHHS report. The report was simply a spreadsheet that listed provider wage information, which the report stated had been collected from state Uniform Financial Reports (UFRs) and from the federal Bureau of Labor Statistics (BLS).
The EOHHS report did show that the average direct-care wage in Massachusetts as reported on provider UFRs was $43,263, or $20.80 per hour, in FY ‘22. That average had increased from $18.38 – or by 13% — from FY ’21.
Those wage averages were lower than BLS median numbers listed in the EOHHS report. The BLS median for FY ’22 was $21.94 per hour. It doesn’t appear that there is any requirement that providers pay the BLS median amount.
Also, based on our own review of UFRs, it doesn’t appear that those reports offer a way to track whether individual providers are actually spending 75% of their state revenues on direct-care wages. The reports we reviewed showed the amounts providers paid in total salary and wages, but did not appear to us to clearly break out the providers’ expenditures on direct-care wages.
We asked OSD for an explanation of the breakdown of expenses under the UFR system. An OSD official referred us to EOHHS, which did not respond to our request.
No directives issued on raising direct-care wages
In January, we also sent two Public Records Law requests to EOHHS and DDS, seeking documents concerning the impact of the Reserve fund on direct-care wages and any directives that have been issued to providers about spending 75% of their reserve account funding on direct-care wages.
In response to our Public Records requests, both EOHHS and DDS stated that they had no records of any such directives; and they provided no records concerning the impact of the reserve account funding on wages.
Healey’s budget doesn’t include wage increase language
It appears that the administration and the Legislature have at least one major difference in their planned approach to addressing the wage problem. Governor Healey’s proposed budgets for FY ’24 and ’25 have not included the provider reserve fund language inserted by the Legislature requiring providers to direct 75% of their funding to direct-care wages.
That language was inserted by the Legislature in the Fiscal ’23 and ’24 budgets. It remains to be seen whether the Legislature will once again insert the language in the FY ’25 budget.
It’s unclear why the governor has not included that language in her budget proposals. A request to the governor’s Office of Constituent Services and to EOHHS for a response to that question about the reserve fund requirement has gone unanswered.
We support higher pay to direct-care and frontline workers. We ourselves have called for a minimum wage of $25 per hour for those workers.
At the same time, we have heard the promises before. Each year, more taxpayer money is given to the providers in line with those promises. DDS-funded group home providers received roughly $1.7 billion this year. Yet, the promises don’t appear to be kept. A few years ago, the state auditor found that those providers were earning surplus revenues as a result of all of that state funding.
We think the state needs to enact tighter controls over the billions of dollars it gives to the providers in order to ensure that they really do honor the promises of higher direct-care wages. To the extent providers are still earning surplus revenues due to funding from the reserve account, the state needs to make sure that the money really is going to direct-care workers and not to executives.
Governor Healey’s proposed FY ’25 budget for DDS raises questions about her priorities for state vs. corporate-run care
Governor Maura Healey last week proposed a budget for Fiscal Year 2025 that includes an increase in funding for the Wrentham and Hogan Intermediate Care Facilities (ICFs) and state-operated group homes in Massachusetts.
But the governor’s budget doesn’t appear to be an attempt to change a longstanding practice of underfunding those state-run services and steadily increasing funding to corporate group home and community-based day program providers.
Healey proposed an increase of only $1.2 million in the ICF line item, which would amount to a funding hike of less than 1%, for FY ’25. That is well under the current average inflation rate for New England of 2.9%. As such, the governor’s budget proposal represents a cut in the ICF line item when it is adjusted for inflation.
Healey’s proposed $15.3 million increase in the state-operated group-home line item would amount to a 4.8% funding boost. While that is above the inflation rate, it is still far less than the governor’s proposed percentage increases in many DDS corporate provider line items.
For instance, Healey is proposing an 18.5% increase in the community-based day program line item, a 19.3% increase for transportation providers, and a 22% increase for respite providers.
Corporate group home cut would be offset by reserve account increase
Healey cut the DDS corporate provider group home line item by $40.3 million earlier this month as part of an across-the-board series of “9C” cuts in the face of a decline in projected revenues in the current fiscal year.
But in her FY ’25 budget, the governor is proposing not only to restore $23.2 million of the $40.3 million cut to the line item, she is also proposing a record-breaking $217 million increase to a separate reserve fund for the corporate providers. The governor’s FY ’25 budget would bring total funding under the Human Services Provider Reserve fund to $390 million.
So it would appear that despite the declining revenues, corporate DDS and other human services providers would receive a net increase of nearly $200 million under the governor’s budget plan.
Questions about provider reserve fund
Last week, The Boston Globe reported that Healey was planning in her FY ’25 budget to “tackle the staffing crisis plaguing social service care providers with a big investment…” That investment appears to include the governor’s proposed $390 million appropriation to the human service provider reserve fund, plus $95 million from a number of other reserve funds.
The total of $485 million in proposed additional funding is projected by the administration to raise direct-care wages to $20 an hour, “at the lowest,” the Globe reported.
We have a number of questions about the oversight of the reserve fund, however. We have long been unable to get answers to those questions, including the amount that has been spent from the fund to actually raise direct-care wages.
Also, for the past two fiscal years, the Legislature has inserted language into the line item for the reserve fund stating that 75% of the funding under the account must be directed to boost direct-care wages. Yet, this language is not included in Governor Haley’s FY 25 proposal for this line item.
Also. the governor’s FY ’25 budget plan indicates that zero dollars were expended in FY ’23 from this same line item that year even though $285 million had been appropriated to it. (See screenshot below.) It’s not clear what has been expended from the line item in the current fiscal year. This raises further questions for us as to where the money in the line item gone.
Minimal increase for ICFs
Gov. Healey’s FY ’25 budget would increase the ICF line item (5930-1000) by $1,777,048, or less than 1% over the current year appropriation. The FY ’25 ICF line item proposed amount is $124,809,632.
We are recommending a $5 million, or 4%, increase in the ICF line item in the FY ’25 budget. That would nominally raise the line item to $128,577,887. That increase would allow the line item to keep pace with inflation moving forward.
The news is better for the state-operated group home line item (5920-2010). The governor’s FY ’25 budget would raise that line item by $15,327,687 or 4.8%. That would raise the line item to $333,099,736.
ICF budget language
We are continuing to recommend changes in the ICF line item language. (The language doesn’t appear to be a part of the governor’s proposed budget. It gets added by the Legislature.)
The legislative language in the current year budget states that DDS must report yearly to the House and Senate Ways and Means Committees on “all efforts to comply with …(the) Olmstead (U.S. Supreme Court decision)…and… the steps taken to consolidate or close an ICF…” (my emphasis). However, closing institutions was not the intent of the Olmstead decision, which was written by the late Justice Ruth Bader Ginsburg.
We are concerned that the misstatements in the ICF line item in the state budget each year could allow the administration to justify continuing to underfund the line item, and possibly to seek the eventual closures of the Wrentham and Hogan centers.
We believe the budget language should be changed to state: “…the steps taken to consolidate or close an ICF and the steps taken to inform families of the choices available for residential care including ICF care.”
Secondly, the legislative line item lists three conditions for discharging clients from ICFs to the community, but leaves out one of the key conditions in Olmstead, which is that “the client or their guardian does not oppose the discharge.” We are requesting that that condition be added to the language in the line item.
In sum, we hope the governor and her staff will begin to understand the importance of state-run services as a part of the fabric of care for persons with intellectual and developmental disabilities. We are seeking a meeting with the governor and her staff to explain the disastrous result if current budget trends are allowed to continue.
Secondly, we think the administration and the Legislature need to understand that adequate oversight is needed of the hundreds of millions of dollars in budget appropriations that are intended to raise direct-care staff wages.
Family thanks DDS commissioner for referral of sister to the Wrentham Center
[Editor’s Note: We are reprinting a letter below that was written by Joan Norman, a sister of Ellen Gallagher. Ellen, who has an intellectual disability, had been living in a corporate, provider-run group home, which was moving to evict her because they admittedly couldn’t meet her needs.
Ellen has Alzheimer’s disease and limited mobility mainly due to limited vision issues and age. Joan describes her as “sweet and social,” but said she had been declining in the group home due the advancement of her disease and “sub-par medical and mental health care.”
In November, after advocacy on Ellen’s behalf by her family and members of COFAR, Department of Developmental Services (DDS) Commissioner Jane Ryder granted Ellen a rare admission to the Wrentham Developmental Center.
The number of residents at Wrentham and the Hogan Regional Center has been steadily declining for several years. That is because a succession of administrations has had a policy of declining to offer Wrentham or Hogan as residential options even when families ask for them.
We think Joan’s letter to Commissioner Ryder is an eloquent testimonial to the quality and importance of the care provided by state-run Intermediate Care Facilities (ICFs) such as the Wrentham and Hogan Centers.]
_____________________________________________________________________________________________
Dear Commissioner Ryder,
This letter is to formally thank you for supporting our sister’s referral to the Wrentham Developmental Center (WDC) back in November.
As you might remember, Ellen Gallagher, a 55-year-old Down Syndrome woman on hospice, with advanced Alzheimer’s, was living in her group home’s family room due to losing the ability to walk or get to her 2nd floor bedroom for almost 4 months.
We fought hard to find the appropriate placement with 24/7 nursing care so that Ellen could live out her remaining time with dignity and proper medical and mental health services. She needs services that include continuity and onsite care, rather than visiting the ER, hospital stays and unnecessary tests when she has had minor issues such as dehydration.
Now that she has settled in at WDC and has spent 6 weeks there, we can confirm it is an amazing living environment where her medical needs are finally being met and she is safe. She now has a handicap accessible bathroom and there are appropriate safety measures to match her abilities and changing needs.
We realize there is a push to keep people out of ICFs like WDC, but for medically complex clients it should be an option and it should be offered willingly by DDS. Families should not have to fight so hard for the care they need. ICFs are not the institutions of the past.
In this case, WDC is an example of the type of culture that is needed in community-based homes where a client’s medical care doesn’t involve neglect, safety issues and unprepared front-line workers.
We suspect costs are a driving factor behind limiting ICF placements. If you look at costs in community-based homes, many medically complex people end up with unnecessary emergent care because they don’t have onsite nursing care. Caretakers (with little to no medical background) use ambulances and hospitals “to be safe” when issues arise. Or worse, many clients go without proper medical care when they need it.
In my sister’s situation, in one incident, she was so dehydrated she ended up in the hospital nearly unconscious for days after being left virtually alone with a COVID infection. The staff handed her over to us after her isolation period, and we took her directly to the ER. She never gained back her strength, and it began a downward spiral of physical and mental decline for her.
In theory, nursing staff should be available to coordinate client medical care in group homes, but that is not how it often works. This can result in sub-par care, but also higher costs for the state’s Medicaid program when emergent care and unnecessary hospitalizations are used in place of qualified medical workers who can properly assess and address medical issues properly.
We urge you to continue supporting families who are seeking placements in an ICF like Wrentham, particularly for medically complex clients. Quality 24/7 medical care is not available in community-based homes, or it is patched together at best. WDC can offer this type of care.
There is a federal regulation supporting the choice of an ICF: Individuals seeking care, and their families and guardians, should be given the choice of either institutional or home and community-based services. [42 C.F.R. § 441.302(d)]. We got our choice for Ellen, and we sincerely thank you for supporting that decision. Please consider supporting others as well.
Sincerely,
The family of Ellen Gallagher